A gradually progressive subsequent spongiofibrosis in urethral will lead to decrease in the diameter of the lumen that cause the stricture. The classification of urethral stricture can be divided into iatrogenic, idiopathic, traumatic and inflammation [1]. There are a few options for management of urethral stricture. The options are based on the causes, sites and severity of the stricture. Urethral dilatation, internal urethrotomy, urethroplasty and urethral stent placement can be considered as line of management for urethral stricture. However high failure rate has been reported for both internal urethrotomy and urethral dilatation [2]. Urethroplasty can be considered as the best option but due to more invasive and technically complex procedure, some patients are unable to go for surgery. As a temporary treatment for urethral strictures, the insertion of a thermo-expandable stent made of a nickel-titanium alloy also known as MemokathTM has been assessed in several studies [3]. The MemokathTM has a “shape memory” feature which is presented in two crystalline forms: the more pliable form and the more rigid form. When the alloy is cooled to same or less than ten degrees of Celsius, the MemokathTM will transform into pliable form. At body temperature or higher, the rigid form holds the memorized shape of the MemokathTM. Most of the MemokathTM studies have been limited to single stent insertion and no studies done for double stents insertion.
Case report
An 81-years-old gentleman presented with recurrent dysuria, incomplete voiding and weak stream for past few years. The symptoms arose after underwent colorectal surgery few years back. He underwent multiple operations since then and the last operation was for internal urethrotomy. Unfortunately, the internal urethrotomy failed and since then he was on urinary catheter. In a few occasions, the urinary catheter was able to be removed but the lower urinary tracts symptoms worsened throughout the years. Subsequently patient developed AUR that required suprapubic catheter (SPC) insertion.
On examination, abdominal wall scars are well healed with no herniation seen. Bilateral kidney not ballotable and bladder not distended. SPC site was clean and no signs of infection seen. There was sedimented urine in urine bag however urine colour appeared clear. There was slit like opening of urethral at the glans penis. No discharge seen from the urethral.
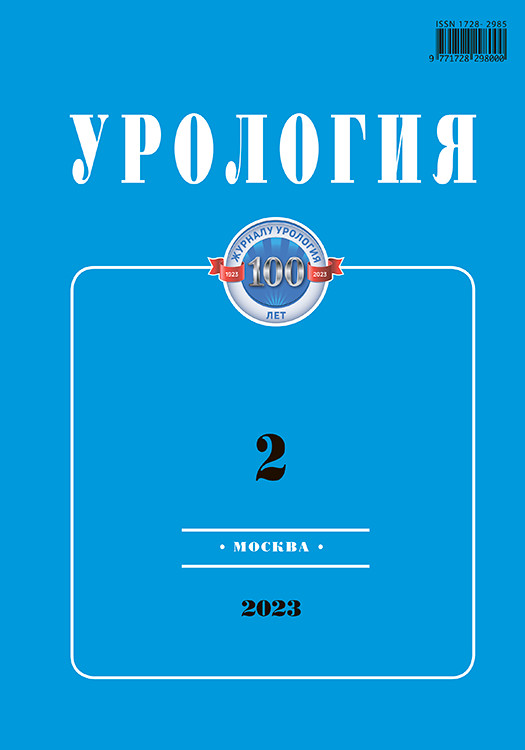
Laboratory investigations including full blood count showed leukocytosis (13.2 x109/l) and presence of leucocytes in urine FEME whereas other biochemistry profiles were within normal limits. Urine cultures reported as Klebsiella Pneumonia Extended Spectrum Beta-Lactamase (ESBL), hence patient was treated with antibiotic according to sensitivity. The MCUG and ascending urethrogram was done and reported as multifocal short segments alternating narrowing and dilatation of penile urethral with beaded appearance. These segments collectively measure 29.01 mm in length as narrowest part measures 2.3mm in caliber (Figure 1). There was hair-line short segment narrowing seen at bulbar urethral measuring 0.9cm in length. There was another short segment narrowing at bulb membranous junction measuring 6.96 mm in length and 2.5mm in caliber (Figure 2). No filling defect, contrast leak or fistula seen in this imaging.
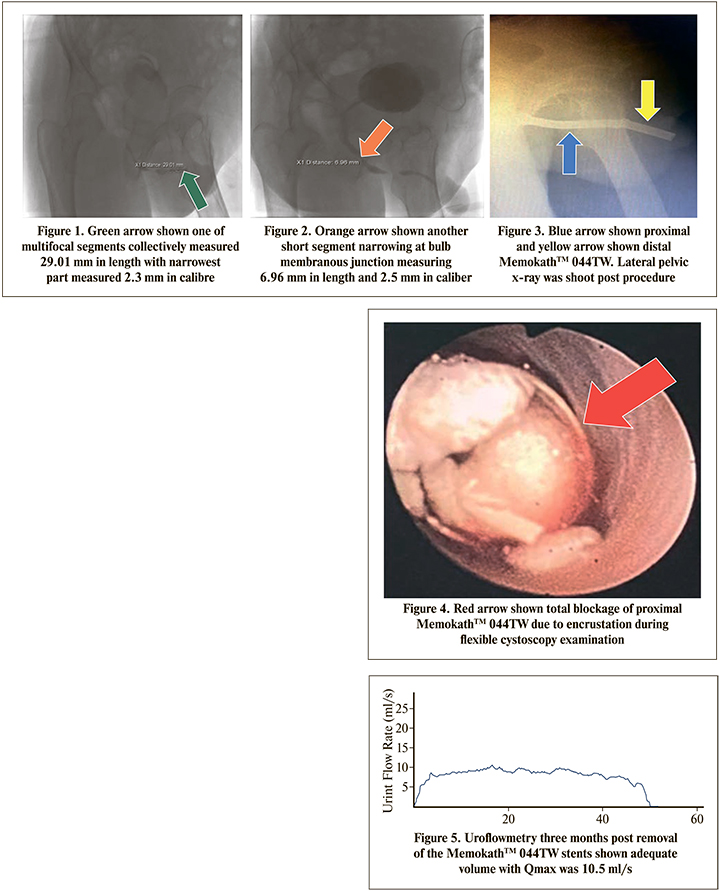
Patient underwent direct visual internal urethrotomy (DVIU), MemokathTM stents insertion and formalization of SPC. Intraoperative findings noted prostate is mildly occlusive, trabeculated bladder wall and whole length stricture over anterior urethral. Two MemokathTM 044TW stents were inserted in anterior urethral. The first MemokathTM 044TW measured 7cm in length placed over bulbar urethral and another MemokathTM 044TW measured 4cm in length placed until distal urethral just before meatus. The formalization done using 14 Fr silicone SPC. Lateral pelvic X-ray done with both stents in situ (Figure 3). Post operation he developed urosepsis that required fluid resuscitation and intravenous antibiotics Cefepime. He fully recovered after five days and able to pass urine through urethral, SPC was removed prior to discharge. One year after the operation, patient came again with recurrent lower urinary tract symptoms and developed AUR that required SPC insertion. Flexible cystoscopy was done and noted there was encrustation at the proximal and distal MemokathTM 044TW stents (Figure 4). Both stents were removed and he still able to pass urine from urethral. SPC was removed prior discharge. Uroflowmetry was done three months post removal of the stents with adequate volume as Qmax was 10.5 ml/s and post void residual (PVR) was 30 mls (Figure 5). He is still under our follow up for his urinary symptoms.
The use of MemokathTM was proven effective to maintain urethral patency in patients which are treated with urethrotomy or dilation [4]. As in our case, the patient underwent DVIU prior the MemokathTM 044TW insertion, hence as mentioned by previous studies the urethral patency was able to be maintained and prolonged the life-span of the MemokathTM itself. Wong et al reported patients remained stricture free after MemokathTM removal [5].
There are few adverse effects related to MemokathTM stenting which are stent dislocation, pain or discomfort, stone encrustation, recurrent strictures with the stent in place and also stent migration [6]. We suspected encrustation inside the lumen of MemokathTM 044TW because patient presented with recurrent lower urinary tract symptoms and ultimately developed acute urinary retention that required SPC insertion. In presented case, patient underwent flexible cystoscopy and diagnosis stent encrustation confirmed endoscopically. According to literature, minor calcifications inside the stent could be managed by lithotripsy. This is to avoid the need for stent removal and to prevent severe stone obliteration [6]. However, in our case, we opted to remove the MemokathTM 044TW stents in view of both stents were calcified with encrustation and patient is not fit for lithotripsy under general anaesthesia due to multiple comorbidities.
Literature reported only using single MemokathTM stent insertion for urethral stricture management. However, many urologists have been using double stents as an option in selected cases. We would like to report the use of double MemokathTM stents as an option for urethral stricture in an unfit patient for urethroplasty. The procedure comes with difficulty due to technical reasons. The MemokathTM is costly and using two stents would be more expensive. Despite the cost, the MemokathTM was reported to last a lifetime if no complications arise. Hence, we offered to patient this option.
Despite being an option and patient was symptom free for twelve months, he presented again with recurrent lower urinary tract symptoms and subsequently developed AUR. During investigation we found patient to have encrusted stents, Martov et al reported a patient with encrusted stent post urethroplasty even after 9 years. [7] We removed both stents as the treatment. Subsequently, patient recovered well and did not require reinsertion of MemokathTM stents. Uroflowmetry was done and showed satisfactory result and did not require further intervention. He had neither recurrent urinary retention nor urosepsis after that.
The MemokathTM was reported to last a lifetime but complications may arise. Only few case reports were reported due to limited experiences and numbers. The literatures are sparse and more studies need to be conducted to evaluate the relation of number of stents inserted with the outcomes. Double urethral stents can be an option for urethral stricture in highly selected cases as it may come with complications.
In conclusion, the MemokathTM stents should be used for highly selected patients. The patients who are medically not fit for urethroplasty, the patients who failed multiple surgeries and the patients who refuse for further surgical management should be considered for the MemokathTM stent insertion. Exchange or removal of the stents may be required due to associated complications. More studies on double stents should be conducted for an alternative option compared to single stent insertion.