Urethral catheters are commonly used in medical practice. It serves as a tool and aids clinicians in managing patients. Well-defined complications are urinary tract infection, bladder injure, urethral stricture or paraphimosis. In rare cases, iatrogenic hypospadias can occur. These complication causes psychological, social, and sexual trauma [1].
The use of urethral catheter for urinary diversion in patients with severe manifestation of COVID-19 can lead to iatrogenic hypospadias. Ventral pressure exerted by the catheter on the delicate urethral meatus causes ischemia and may lead to iatrogenic hypospadias. High suspicion from medical staffs is required to detect and diagnose this condition. It is more common in elderly patients with neurological or musculoskeletal illness [2].
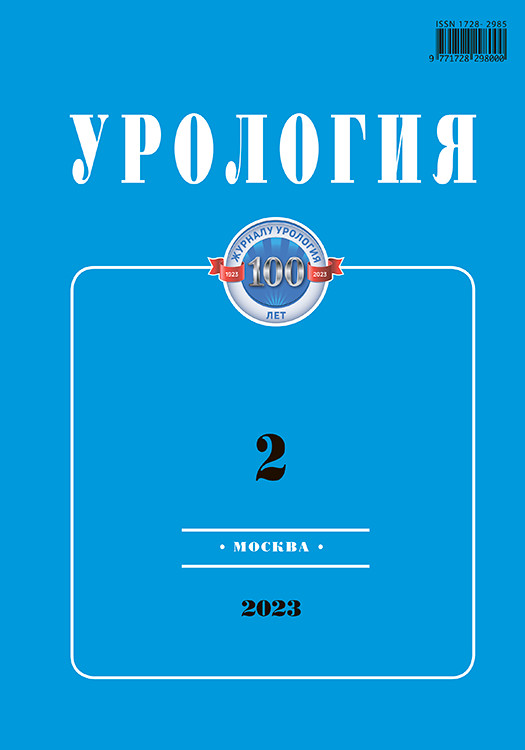
Despite being a rare complication, it is becoming more commonly detected due to increased awareness. Classification of iatrogenic hypospadias by Becker et al in 2018 has been used to classify the condition and to aid in treatment (Fig. 1 and Tab. 1). According to Becker’s classification, our patient had iatrogenic hypospadias of Grade 3. The author suggested for suprapubic tube for Grade ≥2 cases [3].
Case Report
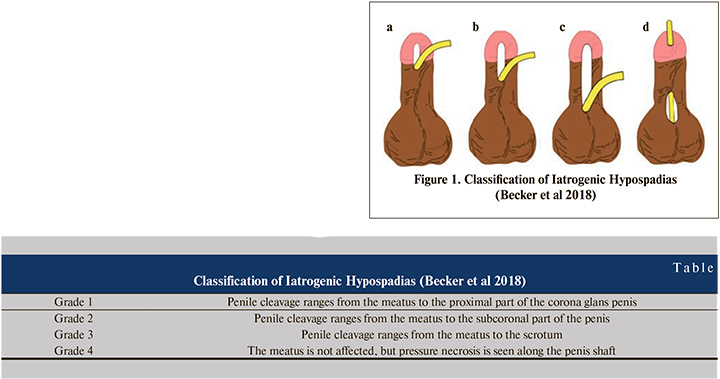
A 32 years-old man with COVID was admitted to the ICU. He was obese and required prone position to maintain respiratory function. Foley catheter was inserted for monitoring of urinary output. Unfortunately, in prone position it was difficult to diagnose a development of iatrogenic hypospadias. Urogenital examination showed eroded penile glans and shaft on the ventral surface with surrounding ulceration and tissue sloughing (Fig. 2). Urine culture showed E. Coli, which was treated with antibiotics. After he recovered well from COVID-19, catheter was removed, and wound dressing was done.
Patient had proximal penile hypospadias with a 4cm defect from the meatus (Fig. 3). He successfully undergone two-stage Bracka urethral reconstruction with 5x3cm buccal mucosa graft (BMG). We had two teams during first stage surgery. A team 1 performed penile reconstruction, while team 2 harvested BMG. Initially, an inverted U-shaped incision done. Urethral plate and margins were freshened. BMG was positioned as new urethral plate with fixing sutures. New urethral plate looked elastic and soft without any scars prior to second procedure, which was done 6 months later to allow good engraftment of BMG at the urethral plate (Fig. 4). During second stage, urethral mucosa was tubularized, and meatal reconstruction and glanuloplasty were done.
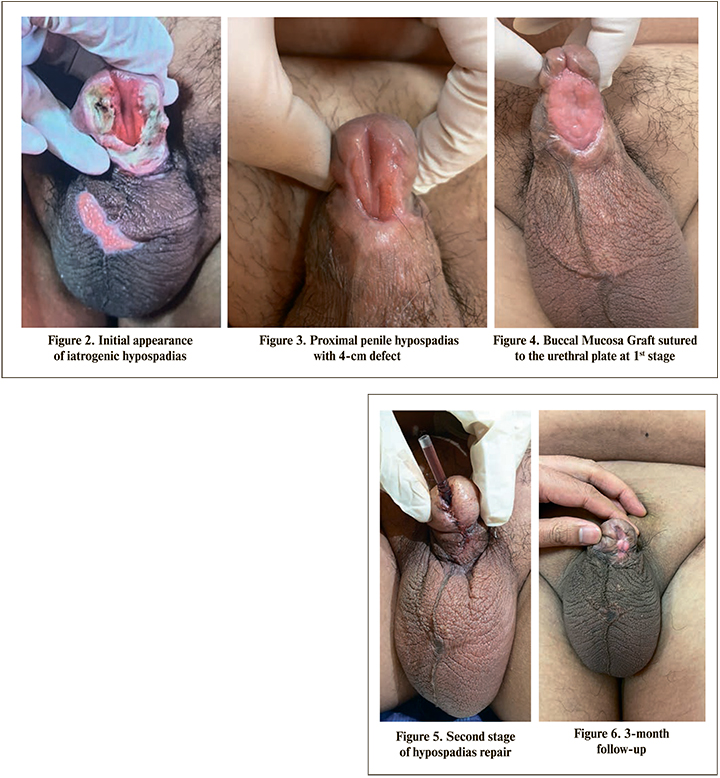
A suprapubic and urinary catheter were held in place for 3 weeks and then successfully removed (Fig. 5). Post-operative period was uneventful. During follow-up, he has good urinary flow, confirmed by uroflowmetry, with no chordee or fistula. Despite superficial skin dehiscence developed, the patient was satisfied with the cosmetic and functional outcome (Fig. 5).
Urinary catheterization is a common procedure performed by doctors and health staff. However, prolonged catheterization is associated with an increased risk of complications. Rare complications such as iatrogenic hypospadias can occur if not timely revealed. It is usually detected late because many specialists have limited experience about this condition. Our patient was a young man with no neurological or musculoskeletal illness; thus, it can happen at any age.
There are less than 50 cases reported in the literature. Barnes-Snow et al. described 3 patients in 1985 and Larsen and Hansen published 2 cases in 1989. Throughout the years, only few articles about this condition were published since it is rare in both adults and pediatric age group. HO Andrew et al. followed 16 patients with iatrogenic hypospadias, which was diagnosed within 3 months to 16 years after catheter removal [4–6].
A repair of iatrogenic hypospadias can be done either with single stage or two-stage technique. Due to limited publication, there is no consensus which option is better. Andrew et al. used single-stage procedure in 6 patients aged 20–47 years old. In a prospective study carried out by Ami Lal Bhat et al. single-stage TIP reconstruction was done in 6 out of 12 patients (9 to 55 years old) with good cosmetic and functional outcomes. However, in older patients a suprapubic tube was put. H Ozturk performed Mathieu repair in 16 years old boy with good cosmetic outcome [7–9].
Our center has experience using BMG for urethroplasty and two-stage procedures for re-do adult hypospadias. Outcomes are good and favorable. This is our first experience treating iatrogenic hypospadias, hence we proceeded with two-stage procedure with BMG. Other factors which were in favor of two-stage technique were penile length, shape of glans, meatal size, poor quality of the urethral plate and difficulty for urethral tubularization when single-stage procedure is performed. However, no publication dedicated to two-stage technique was found.
Younger patients would benefit from definitive surgery to obtain good urinary and sexual function with acceptable appearance. Our patient was young; thus, reconstructive procedure was the preferred option. In the future, more data on iatrogenic hypospadias can be reviewed. However, prevention is always better than treatment. Other options of surgical reconstruction can be explored for obtaining better outcome in different scenarios.
Iatrogenic hypospadias is a preventable complication in patients with indwelling urethral catheters. It is a devastating complication, which can be prevented with good care and early catheter removal. A reconstruction should be offered and performed for younger patients to ensure good function with acceptable penile appearance. Surgical treatment will improve psychological, sexual, and social outcomes.